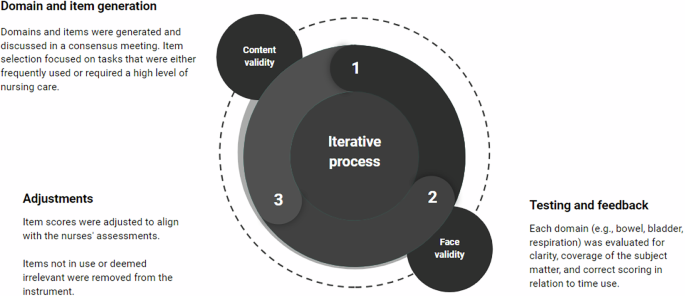
In the present study, we have developed and evaluated a tool for care intensity assessment at a highly specialized SCI rehabilitation unit. The tool was developed and evaluated through an iterative process involving three main steps. The steps involved securing feasibility, face validity, content validity, and testing the reliability. Through in-depth discussions among nurses, we sought to ensure that each item within the tool resonated with the core nursing needs of patients with SCI. The first part of the process revealed different perspectives e.g., some advocated for a comprehensive array of items to capture the nuanced complexities of patient care, while others emphasized the necessity of efficiency and alignment with the primary aim of the tool. Striking a balance between these competing demands was paramount, ultimately culminating in a refined version comprising 17 items categorized into five levels of nursing assistance.
To our knowledge, this study is the first to develop a SCI specific tool for identifying inpatient care needs in a hospitalized rehabilitation setting. There exists a variety of complexity classification tools within different genres of healthcare. We developed our tool with inspiration from the Rehabilitation Complexity Scale Extended (RCS-E) [15]. The RCS-E was initially designed to identify the clinical need for higher-level services as opposed to local services, especially within neurorehabilitation [22]. Since its initial development, the RCS-E has undergone further adjustments. While its discriminative purposes are highly relevant for referral and it includes important descriptive elements for rehabilitation, it primarily identifies the different professions and specialties that must be present. Therefore, it still overlooks specific areas of special care needs within the daily clinical practice of SCI rehabilitation. Whereas the RCS-E determines if the patient is in the appropriate department, our tool focuses on how to effectively distribute resources to meet patient needs. Additionally, our tool may also be further developed for referral purposes. The area of palliative care has also been subject to similar tools. A systematic review from 2021, investigated systems for the complexity of patient care needs, however, their findings were primarily targeted at identifying complexity in primary care and were used to address the care requirements of the individual for engaging appropriate resources and managing health service planning (e.g., for referral purposes similar to RCS-E) [23]. Other important classification tools include functional measures such as the Spinal Cord Independence Measure (SCIM) [21], which assesses the functional level of individuals and is routinely used within SCIWDK. However, the functional level does not necessarily translate into specific care needs and may not consider other critical components, such as psychological well-being and pain management. While a functional score provides valuable information for e.g. rehabilitation purposes, it may be insufficient for capturing the full spectrum of a patient’s needs. Therefore, care needs and functional scores can complement each other and could be considered for combined use in the future to provide a more comprehensive assessment of patients. A next step could be investigating the concurrent validity between the NCA-SCI and SCIM to determine how well these tools correlate and enhance the overall evaluation of patients’ needs.
Another area is the assessment of workload within clinical settings, as investigated in a review by Racey et al. [24]. Nursing workload can be affected in various ways, such as the time spent at the bedside with a patient, the competency level of the nurse, and the complexity of the care delivered; these measures describe another aspect of care needs [25]. With resource shortages, the workload and mental well-being of staff are at risk. In this context, our tool becomes essential for effectively balancing care needs and available resources. Further, the NCA-SCI tool can serve as a foundational framework for creating a common language among healthcare professionals when discussing patients and their care needs. By providing standardized criteria and categories, the tool can facilitate clear and consistent communication across multidisciplinary teams. This common language may ensure that all team members have a shared understanding of each patient’s condition, which is critical for coordinated care planning and delivery. A shared understanding may also enhance task-sharing among healthcare professionals. It may help delineate roles and responsibilities, ensuring tasks are delegated according to each professional’s expertise. By categorizing patient needs, the tool enables efficient allocation of routine tasks to support staff, allowing specialized clinicians to focus on complex care. It may also support flexibility and adaptability in dynamic healthcare settings, allowing for quick reassessments and adjustments to care plans.
Strengths and limitations
Our quest for face validity underscored the iterative nature of tool refinement. Through multiple rounds of adjustments based on feedback from clinical settings, we fine-tuned the instrument to encompass relevant themes, enhance comprehensibility, and ensure accurate scoring of time use. This iterative process, spanning ten versions, exemplifies our commitment to refining the tool until it achieved initial agreement. Further, our exploration of agreement between the instrument and nurses yielded insights into the reliability and validity of our assessment tool. Initially, the high prevalence of false answers underscored the need for refinement. However, through meticulous adjustments to item scores and text, coupled with simplification efforts to minimize misinterpretation, subsequent rounds revealed significant improvements.
In the agreement between raters’ we only included four persons, however the results may still be indicative. Overall, the inter-and intra-rater reliability reached moderate levels, indicative of acceptable consistency in assessing care needs. The moderate Kappa values suggest that while the tool is generally reliable, there are some inconsistencies that could be addressed. Variability in raters’ interpretations and the subjective nature of the assessments might contribute to these discrepancies. Additionally, the 14-day interval between test occasions may have influenced the results, as it allows for potential real changes in patients’ conditions within an inpatient rehabilitation setting. This interval was selected to balance practical considerations, such as minimizing recall bias and accommodating clinical scheduling constraints. Further training and refinement of the tool could enhance reliability. In practice, establishing standardized procedures for patient assessments, including the frequency and the assessors involved, is crucial. Experienced assessors may enhance reliability over time, and more frequent assessments could improve validity and overall usability. However, these improvements should be balanced with available resources. When examining the confusion matrices for both inter- and intra-rater reliability, misclassifications primarily occur between adjacent categories. This pattern indicates a tendency toward ‘minor’ misclassifications, suggesting a low risk of incorrectly classifying an E as a B or vice versa, and thus a minimal risk of major clinical misinformation.
We only included nurses and one occupational therapist, which may have resulted in the inclusion of items and themes primarily relevant to these professions. As rehabilitation efforts highly rely on interdisciplinary teams, our approach could have benefited from including more professions in the development phase to create a more comprehensive and interdisciplinary tool. Lastly, the tool was specifically developed and tested within the context of SCIWDK and, hence, is currently applicable only within this context. However, we believe that the tool may be easily adjusted to use in other SCI rehabilitation wards and potentially also other medical specialties.
link