Danish eye care system
The Danish healthcare system is universal and based on principles of free and equal access to healthcare for all citizens [18]. General ophthalmologists maintain a gatekeeper function to the secondary sector (general eye departments or university eye clinics). Danish citizens have the right to schedule an appointment with general ophthalmologists independently, with or without a referral from a general practitioner or optometrist [19]. There are currently 430 ophthalmologists in Denmark, of whom 180 are general ophthalmologists and 250 are employed in the hospital sector [8, 20]. With approximately 5.9 million inhabitants in Denmark, this corresponds to 0.7 ophthalmologists per 10,000 inhabitants, which is a little below the European average of 0.8 per 10,000 inhabitants [21]. General ophthalmologists provide care for approximately 3800 unique patients annually [22], a number that has grown over the last 15 years, especially in rural areas, where waiting times are highest [23]. According to the Danish Health Agency, the number of ophthalmologists must be increased by 40–60% over the next 20 years to maintain current service levels [8].
The density of optometry stores in Denmark is among the highest in Europe and it is approximately three per 10,000 inhabitants [24].
Organization of a future OTRP system
Two organizational models are particularly relevant for integrating OTRP services in the Danish public healthcare system: a reimbursement (R-OTRP) model and a public procurement (P-OTRP) model.
A reimbursement model is a common way of integrating general ophthalmologists and other private healthcare specialists in the Danish primary care sector. It could be extended to include both optometrists and teleophthalmologists [25]. It is the model currently used for optometrists in many UK National Health Service trusts and for reimbursing private providers under Medicare or Medicaid in the USA. In Denmark, medical specialists and other healthcare professionals can apply for authorization and permission to work under the Danish Health Insurance Act [26]. These professionals can purchase a provider license which gives them the right to practice within a specific geographic domain and up to a certain capacity (or annual cost level) determined by the regional health authority. After receiving the license, the regional health authority is required to compensate for the services provided to patients in accordance with the nationally agreed contractual terms, which include a fee-for-service schedule. The nationally agreed terms of the contract are determined through negotiations every two years between the relevant specialist organization and the public payers. The provider license is typically open-ended with periodic reviews. An advantage of this model is the life-long relationship between payer and provider that enables monitoring and learning. This health economic evaluation assumes that the R-OTRP model is extended to optometrists and teleophthalmologists. We assume that Danish optometrists under an R-OTRP model can achieve the same level of efficiency as UK optometrists through continuous learning and control [12, 14, 15, 27]. We also assume that both optometrists and teleophthalmologists will receive a tariff for their referrals.
A public procurement or tender model is an alternative model used by Danish health authorities. This model is used regularly by Danish health authorities to buy additional capacity for cataract surgery among private ophthalmologists with or without provider licenses [27, 28]. It is also used to procure ambulance services in each of the five regions through competitive bidding between invited private and public service providers for four-year contracts [29] and it is used to create analog competition for hospital pharmaceuticals [30]. The main advantage of a public procurement model is the possibility of price reductions and financial savings on public healthcare budgets through market competition and the flexibility to adjust healthcare capacity to meet temporary fluctuations in demand [31]. In Denmark, the procurement model can be used at the national or regional level following the Danish Public Procurement Law [32] and Procurement Directives from the EU Commission [33]. The duration of the procurement contracts is typically a fixed period, such as one to four years, and winners may be paid for services in different ways according to specific contractual terms. In this economic evaluation, we assume that competitive tenders could be attractive for various partnerships between optometrists and ophthalmologists e.g., optometrists in stores working together with private ophthalmologists (with or without reimbursement contracts with Danish regions), optometrists working with ophthalmologists in hospitals, and general ophthalmologists who employ optometrists. We assume that the P-OTRP model is likely to be cheaper than the R-OTRP model due to price competition, but that the quality of the eye examinations in stores may be higher in the R-OTRP model because of the continuous working relationship between healthcare providers and the optometrist. For simplicity, we further assume that there is only a single fee paid per referred patient under the P-OTRP model covering services performed by a teleophthalmologist and an optometrist.
Decision-analytic model
A decision-analytic model (a decision tree) with a one-year time horizon was constructed to portray alternative future patient referral pathways for people examined in optometry stores for suspected ocular posterior segment eye disease. The model starts with people having a comprehensive eye examination in an optometry store and ends with the start of treatment or the end of the referral pathway. The model compares three alternative patient referral pathways (Fig. 1): (1) the usual general ophthalmologist referral pathway (GO-RP), where optometrists are not reimbursed by the regional health authorities for the eye examination but refer all patients without any involvement of a teleophthalmologist to a general ophthalmologist, (2) an R-OTRP model, and (3) a P-OTRP model, as described in section 2.2.
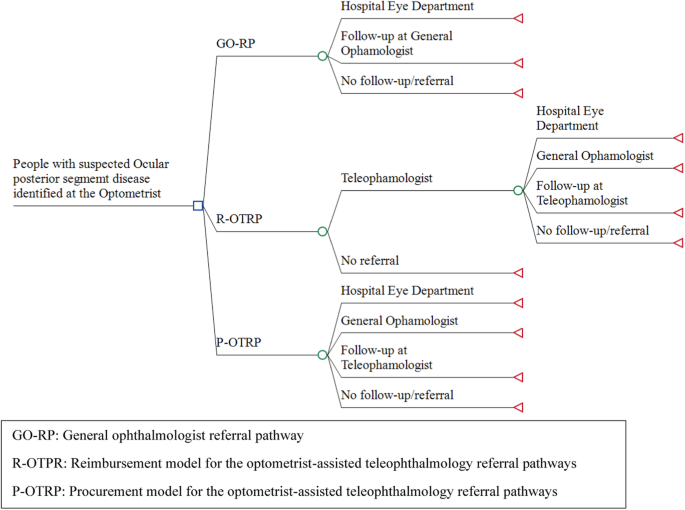
GO-RP: general ophthalmologist referral pathway, R-OTRP: reimbursement model for the optometrist-assisted teleophthalmology referral pathways, P-OTRP: procurement model for the optometrist-assisted teleophthalmology referral pathways, OTRP: optometrist-assisted teleophthalmology referral pathway. For all arms in the model, people with suspected ocular posterior segment eye disease were expected to have their initial comprehensive eye examination in the optometry store. Under GO-RP, patients are referred directly to an ophthalmologist based on the results of the eye exam. Under P-OTRP, the results of the comprehensive eye exam are forwarded digitally to the teleophthalmology service who provides the optometrist with a description of the clinical findings and provides a follow-up/referral plan for each patient, and refers patients to specialized eye care providers. Under R-OTRP, the optometrists are assumed to be able to reduce the number of referrals to the teleophthalmologist compared to P-OTRP (hence the extra branch “no referral”).
The economic evaluation was conducted from a Danish public health sector perspective with the main outputs being total healthcare costs per patient, average waiting time from eye examination in store until the start of treatment or end of referral pathway, and quality-adjusted life-years (QALY) gained. The QALYs were calculated as the difference between the gain in health-related quality of life (HRQoL) from initiation of treatment minus any disutility from potential anxiety during waiting time. As a sensitivity analysis, we included a societal perspective to explore the consequences for patients in terms of transportation and productivity costs. The model was constructed using TreeAge Pro Healthcare (version 2022, R2.0) following international guidelines for health economic evaluation [34, 35].
Model inputs
The model was parameterized using the best available evidence relevant to the model (Table 1). Central model assumptions were validated using an independent expert panel, comprising three general ophthalmologists, two optometrists, and one associate professor of health economics.
The assumptions about cohort disease prevalence were taken from Muttuvelu et al. [11]. We assume the same share of patients with eye disease and the same share of patients referred to treatment at a hospital eye department and general ophthalmologist for all three alternatives (GO-RP, R-OTRP, and P-OTRP) i.e., the clinical quality is assumed not to be affected by the introduction of teleophthalmologist and choice of organizational form.
In the base-case, we assume that all patients in GO-RP see a general ophthalmologist if an optometrist gives the patient a diagnosis after a comprehensive eye examination, but in the sensitivity analyses, this assumption is relieved down to 50%. In base-case analysis for P-OTRP, we assume that teleophthalmologist can reduce the number of referrals up to 80.5% [11], which is varied in the sensitivity analysis from 50–90%. In base-case of R-OTRP, we assume that optometrists can reduce the number of referrals to teleophthalmologist by 10% compared to P-OTRP, which is increased in the sensitivity analysis up to 20%.
All monetary outcomes were estimated in Danish Krone (DKK) adjusted to the year 2022 using the Consumer Price Index [36] and subsequently converted to 2022 British Pound Sterling (£) using a conversion rate on December 12, 2022 of DKK 100 = £11.57. Healthcare costs were obtained from published sources, including the Danish diagnosis-related groups tariff system [37] and tariffs from the Danish ophthalmologists’ collective agreement [38]. The costs/tariffs of teleophthalmologists and optometrists were estimated in base-case to be £46 (DKK 400) and £20 (DKK 175) respectively. The model only includes marginal costs of services from providers, and no attempts have been made to include administrative costs of establishing and running a OTRP system such as the costs of tendering quality assurance or reimbursement. Nor have any potential changes in the costs of implementation been included.
Data on current waiting times in the Danish eye care system were incorporated as average weeks of waiting time for general ophthalmologists and hospital eye departments according to available Danish statistics and validated with the expert panel [20].
QALY gain was included within the one-year horizon as the gain from initiation of treatment of eye disease assuming an increase in HRQoL of 0.2 measured on an EQ-5D scale [39]. The disutility from potential anxiety in the waiting time from eye examination and optometrist’s diagnosis and the start of treatment (for people with confirmed diagnosis) or ophthalmologist diagnosis (false positives) was included, assuming a difference in HRQoL of the average referred patient measured on an EQ-5D scale of 0.02 [39].
Furthermore, the main results are shown graphically in a cost-effectiveness plane constructed from a probabilistic sensitivity analysis with 10,000 2nd-order Monte Carlo simulations using beta distribution for probabilities and QALYs, and gamma distributions for costs and waiting times [40]. In the sensitivity analysis, patients’ transportation costs were included, assuming an average transport cost per consultation at the general ophthalmologist and hospital eye department of £11.75. We further included productivity costs due to patients’ absence from work because of eye consultations, assuming an average cost per consultation at the general ophthalmologist and hospital eye department of £20.83 [34].
link

