Introduction
Eye care service utilization (ECSU) is essential for preventing vision loss, maintaining eye health, and ensuring timely management of ocular conditions (1, 2). However, ECSU rates vary significantly worldwide due to differences in healthcare accessibility, socioeconomic conditions, and awareness, ranging from 18 to 90% (2, 3). High-income countries, such as the United States, Australia, and Canada, report utilization rates between 60 and 90%, largely due to well-established healthcare systems and strong preventive care policies (3, 4). In contrast, ECSU remains much lower in resource-limited settings, with rates of 22% in low-income countries, 24% in lower-middle-income countries, and 37% in upper-middle-income countries (5). Similarly, ECSU in Ethiopia remains low, with notable regional variations; 21.1% in Northern Ethiopia (6), 21.6% in Southern Ethiopia (7), and 32.98% in Central Ethiopia (8), underscoring the need to identify key barriers and improve service delivery across different regions.
The consequences of low ECSU are far-reaching, fueling the global rise in visual impairment and blindness (9, 10). In Ethiopia, vision loss imposes a significant economic strain, with both direct costs like medical expenses and indirect costs, such as lost productivity (11, 12). Nearly one in 10 adults over 60 suffer from visual impairment, much of which could be prevented with routine eye exams (13). Despite strong recommendations from organizations like the American Academy of Ophthalmology, financial barriers, limited eye care services, and lack of awareness continue to hinder ECSU in many low- and middle-income countries (14, 15). As a result, millions remain at risk. Globally, 36 million people are blind, 217 million face moderate or severe visual impairment, and 188 million have mild vision loss (16). Alarmingly, nearly 40% of blindness cases could have been prevented with timely screening and treatment (17).
Despite extensive search on ECSU in Ethiopia, most studies have focused on individual-level factors such as age, income, and health insurance, with limited attention to structural and environmental barriers at the community level. In rural districts like Andabet, where healthcare infrastructure is sparse and long distances to eye care facilities pose significant challenges (18–20), understanding how these factors influence ECSU is critical. This study bridges that gap by incorporating both individual and community-level factors through multilevel mixed-effect analysis, providing a more thorough understanding of access disparities. Unique challenges in the district including limited access to transportation and healthcare infrastructure, compounded by cultural beliefs and traditional practices underscore the urgent need to investigate local cultural influences on ECSU and develop tailored interventions to address them. By emphasizing these localized challenges in line with the World Health Organization’s (WHO) Universal Eye Health Action Plan, the study will advocate for decentralized eye care solutions and offer actionable, context-specific recommendations for Ethiopian policymakers and healthcare planners. More generally, it will provide a scalable model for other low-resource settings, helping to reduce preventable vision impairment and promote universal eye health.
Methods
Ethics statement
This study was conducted following the principles of the Declaration of Helsinki and received ethical approval from the Institutional Review Board of Debre Tabor University, Health Science College (Reference Number: 1099). Additionally, permission was granted by the Andabet District administrative office. Written informed consent was obtained from all voluntary participants, who were reassured that their participation posed no risk of harm. To safeguard confidentiality, personal identifiers were omitted, and unique codes were used to anonymize the data.
Study design and settings
This community-based cross-sectional study was conducted among older adults aged 40 years and above from May 1–30, 2024, in Andabet District. Located 150 km from Bahir Dar, the capital of the Amhara National Regional State, and 717 km from Addis Ababa, Ethiopia’s capital, Andabet spans a vast geographical area with a notably high population density. According to the 2021 regional census, the district has an estimated total population of 153,694, distributed across 35,875 households within 26 kebeles. The district is served by a primary healthcare center and two health posts, providing essential medical services to the community.
Study population and eligibility criteria
The source population for this study included all older adults aged 40 years and above residing in the Andabet District. We included individuals who were 40 years or older and had lived in the study area for at least 6 months.
Sample size determination and sampling procedure
The required sample size was determined using the single population proportion formula, drawing on findings from a similar study conducted in Hawassa, Ethiopia, which reported a prevalence of 23.8% (9). Accounting for a 95% confidence level, a ± 5% margin of error, a design effect of 2.0, and an additional 10% to accommodate potential non-responses, the final sample size for this study was determined to be 612.
Multistage sampling was used throughout the sampling process. First, six kebeles were randomly chosen from a list of 26 provided by the Andabet District Administration Bureau using a simple random sampling method. To ensure representativeness, the sample size for each selected kebele was determined by population proportional allocation. Next, a systematic random sampling technique with an interval of 8 was applied to select households. The first household was chosen using a lottery method, followed by the selection of every Kth household thereafter (K = N/n, where N = 4,881 and n = 612). Before initiating the sampling, a pen-spinning technique was used to determine the starting point. In households with multiple eligible individuals, one participant was randomly selected using a lottery method.
Operational definition
ECSU
An individual was classified as having a good level of ECSU if they reported visiting an eye care facility for a checkup or examination at least once within the past 2 years (8).
Older adults
Individuals aged 40 years and above. They were selected because they face a higher risk of vision impairment and ocular diseases. They are also more likely to require eye care services, yet often encounter significant barriers to access, especially in low-resource settings like Andabet (8).
Data collection tools and procedure
The data collection tool was developed based on a comprehensive review of the existing literature. A pretested structured questionnaire was used to gather data through interviewer-administered surveys, covering sociodemographic details (e.g., kebele, age, sex, residence, religion, education, and occupation) and medical factors such as health insurance status, diabetes, hypertension, proximity to eye care services, use of traditional eye medicine, and ECSU. Four data collectors, all BSc Optometrists, conducted the interview under the supervision of an MSc Optometrist. The collected data were then organized in an Excel format (Supplementary Table S1).
Data quality control
To maintain consistency, the data collection tool was first developed in English, translated into the local language (Amharic), and then back-translated into English. Subsequently, data collectors and the supervisor underwent 2 days of training on data collection procedures. A pre-test was conducted on 5% of the total sample size in a different kebele that was not part of the main study. Based on the pre-test findings, the questions were revised and refined. Supervisors and investigators then reviewed the data to ensure coherence, accuracy, and clarity.
Data processing and statistical analysis
Data entry was performed using Epi-Data version 4.6, while STATA 16 was used for data cleaning, coding, and analysis. To identify factors associated with ECSU, a multilevel mixed-effects logistic regression, accounting for the hierarchical nature of the data, where older adults were grouped within clusters. Multilevel analysis is particularly suited for such nested data structures, as it addresses key assumptions that standard logistic regression does not. Unlike standard models, which assume independence among observations, multilevel analysis accounts for clustering, where individuals within the same group may share similar characteristics. It also incorporates random effects, allowing for variability both within and between clusters, whereas standard logistic regression assumes fixed effects. Additionally, multilevel models recognize that variance may differ across groups, addressing the equal variance assumption of standard models. By considering these factors, multilevel analysis improves the accuracy of statistical inferences when dealing with hierarchical data.
Initially, a bivariable multilevel logistic regression analysis was conducted, and variables with a p < 0.20 were selected for the multivariable multilevel analysis. During the multilevel binary logistic regression, both random and fixed-effect models were fitted. The intraclass correlation coefficient (ICC), a random effect parameter, used to measure the degree of variability in ECSU across clusters. An ICC >10% indicated the importance of considering cluster-level variability, thereby making multilevel analysis absolutely crucial. Additionally, proportional change in variance (PCV) and median odds ratio (MOR) were assessed. Multicollinearity was tested using the variance inflation factor (VIF), with all independent variables showing a VIF of less than five and a mean VIF of 1.85, indicating no significant multicollinearity among the variables.
In the fixed-effect analysis, four models were fitted: model 1 (without explanatory variables), Model 2 (including only individual-level factors), Model 3 (including community-level factors), and Model 4 (incorporating both individual and community-level factors). Of these models, Model 4 was identified as the best-fit model due to its lowest deviance and highest PCV. The adjusted odds ratio (AOR) with its 95% CI was presented for each fitted model, but interpretations were based solely on the final, best-fit model. Variables with a p < 0.05 in the multivariable multilevel analysis were considered significantly associated with ECSU.
Result
Socio-demographic characteristics of study participants
A total of 570 adults aged 40 and above participated in this study, with a response rate of 93.14%. More than half (52.11%) were between 55 and 64 years old, with a mean age of 59 ± 5. Among the participants, 286 (50.18%) resided in rural areas, and 46.67% were engaged in farming. Regarding family monthly income, approximately three-quarters (75.43%) earned <4,000 ETB (Table 1).
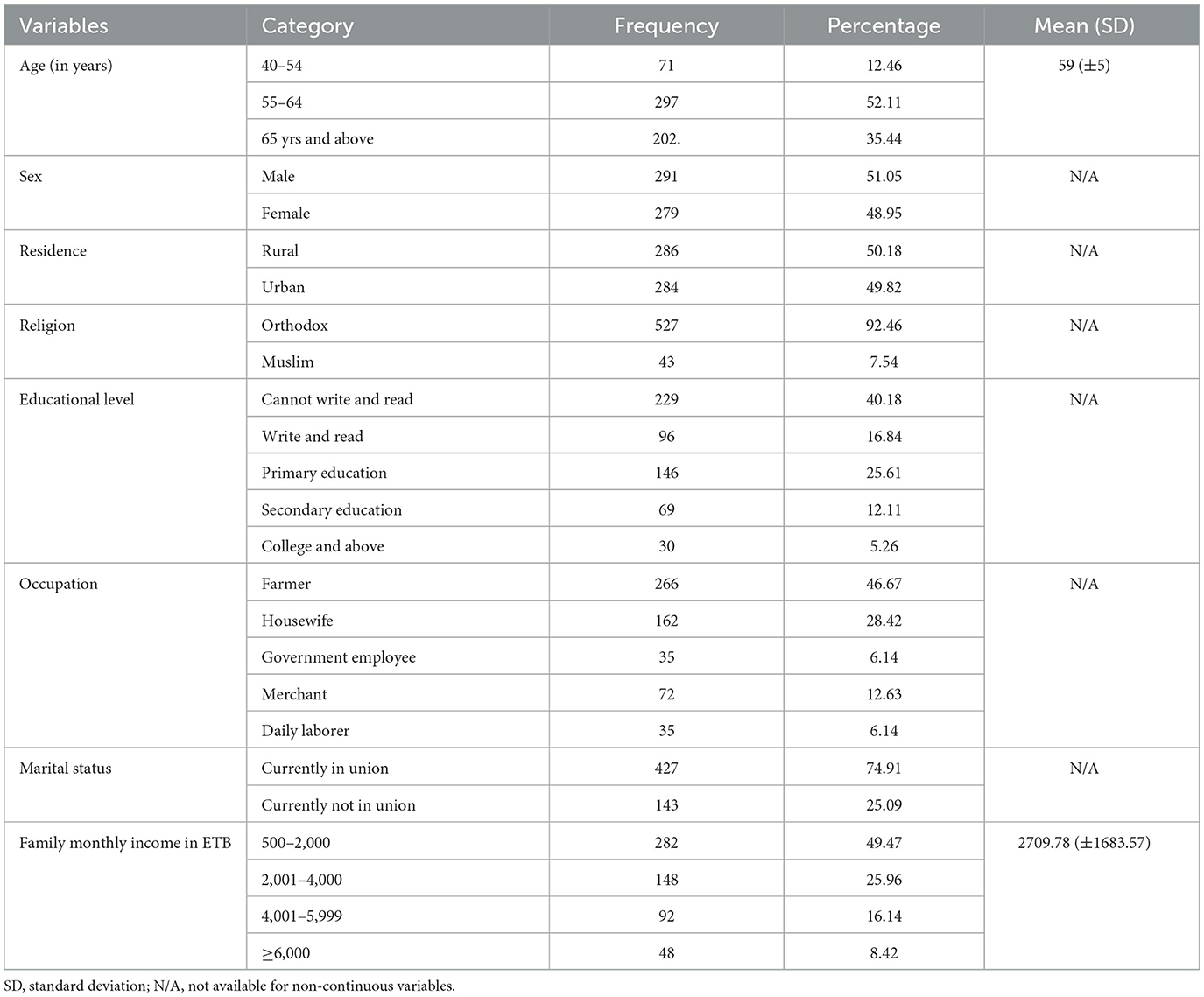
Table 1. Socio-demographic characteristics of older adults in Andabet, Northwest Ethiopia: a multi-level mixed-effect analysis (n = 570).
Medical and related characteristics of study participants
A total of 254 participants (44.64%) had a history of eye diseases. Among them, nearly half (47.25%) reported that their eye condition affected their daily activities. However, the majority (89.12%) were unaware of the importance of regular eye checkups, and approximately half (48.07%) lived far from healthcare facilities (Table 2).
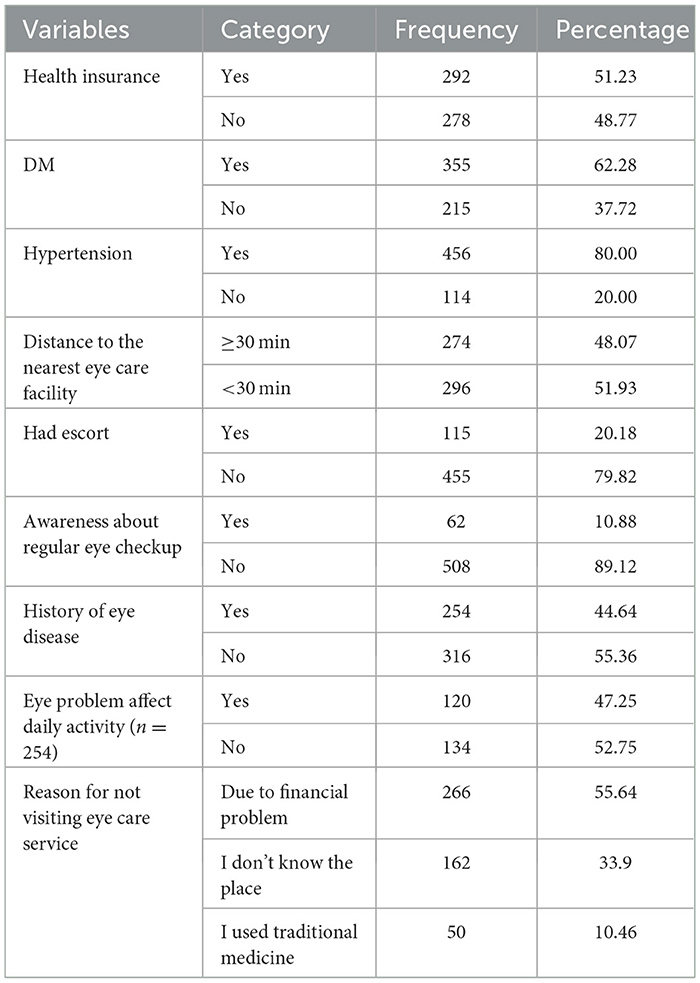
Table 2. Medical and related characteristics of older adults in Andabet, northwest Ethiopia: a multi-level mixed-effect analysis (n = 570).
Eye care service utilization
This study revealed that 16.14% (95% CI: 13.11, 19.16) of participants had a good level of ECSU, while the remaining 83.86% had a poor level.
Model fitness
In the random-effect analysis, Model 1 showed that around 70.3% of the total variation in ECSU was observed at the cluster level and attributed to community-level factors. Moreover, Model 1 had the highest median odds ratio (MOR) of 14.15, indicating that individuals in a kebele with a higher risk of poor ECSU were 14.15 times more likely to experience poor ECSU compared to those in a lower-risk kebele. Additionally, the final model (Model 4) had the highest proportional change in variance (PCV) at 88%, demonstrating that both individual and community-level factors explained 88% of the variation in ECSU across communities. Model fitness was assessed using deviance, and Model 4, which exhibited the lowest deviance, was determined to be the best-fitted model (Table 3).
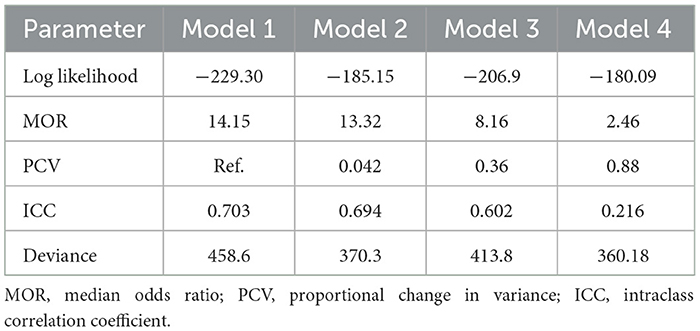
Table 3. Random effect and model fitness of eye care service utilization and associated factors in Andabet district, northwest Ethiopia: a multi-level mixed-effect analysis (n = 570).
Factors associated with eye care service utilization
In multivariable multilevel logistic regression analysis, where both the individual and community level factors were fitted simultaneously; age, health insurance, distance to the nearest eye care facility, and awareness about regular eye check-ups were significantly associated with good level of ECSU.
Individuals in the age group of 65 and above were 4.59 times more likely to utilize eye care services (AOR = 4.59; 95% CI: 1.38, 15.21) as compared to individuals in the age group 40–54 years. Similarly, Participants who had health insurance were 1.98 times more likely to utilize eye care services (AOR = 1.98, 95% CI: 1.51, 2.58) as compared to their counterparts. Regarding distance to the nearest eye care facility, Participants living nearer to the eye care facility were 6.42 times more likely to utilize eye care service (AOR = 6.42, 95% CI: 1.95, 21.15) as compared to their counterparts. In the same manner, the odds of using eye care service from participants who had awareness about regular eye checkups were 1.63 (AOR = 1.63; 95% CI: 2.88, 9.70) times higher than their counterparts (Table 4).
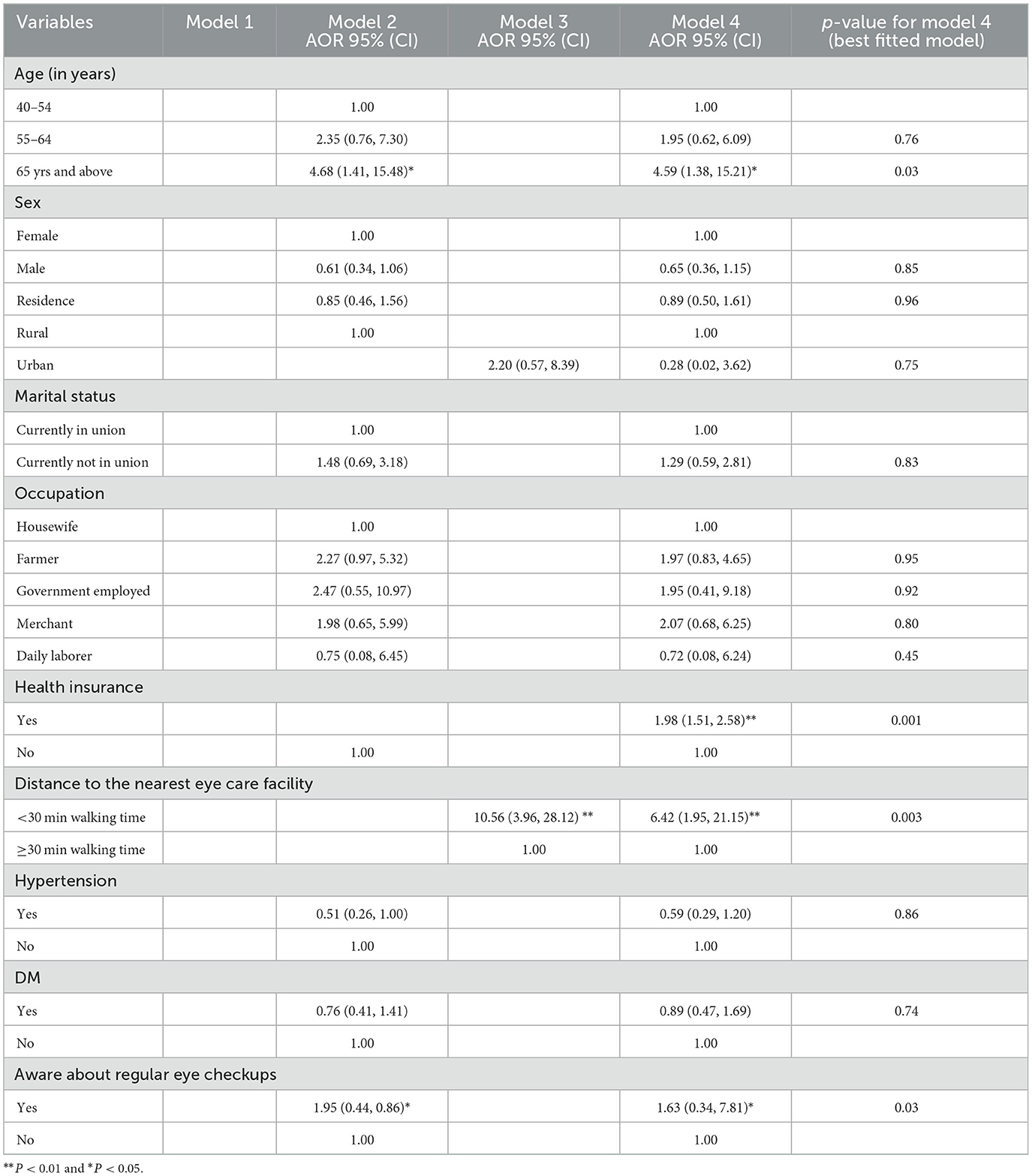
Table 4. Multi-level mixed-effect logistic regression analysis for factors associated with eye care service utilization among older adults in Andabet district, Northwest Ethiopia (n = 570).
Discussion
This study found the magnitude of ECSU to be 16.14%, a rate consistent with studies conducted in Northwest Ethiopia (6), Gamo Gofa [Southern Ethiopia; (7)], and Yobe, Nigeria (21). This similarity may stem from comparable healthcare access and sociodemographic factors, such as education level and income (22). Specifically, in these Ethiopian local regions, lower education levels and economic constraints may limit awareness and affordability of eye care services, resulting in similar utilization patterns (23). However, this magnitude of ECSU was found to be lower compared to different studies conducted in Hawassa (9), Debre Birhan (8), Gondar (24), Ghana (25), Edo state of Nigeria (9), Abuja Nigeria (26), Limpopo province of South Africa (26), United States (27) and Australia (28). Several factors may explain this difference, including variations in healthcare infrastructure, socio-demographic characteristics, and cultural influences (29). Urban Ethiopian areas like Hawassa, Debre Birhan, and Gondar typically have better-equipped healthcare facilities, a higher concentration of trained eye care professionals, and more specialized services compared to rural areas, which likely contributes to higher utilization rates (30). Additionally, the findings from studies conducted outside Ethiopia may be influenced by socio-demographic factors such as higher income levels, better socioeconomic conditions, and more established health systems, all of which contributed to greater healthcare utilization. In contrast, economically disadvantaged populations, particularly in rural Ethiopia like Andabet, often face challenges such as high out-of-pocket costs, limited transportation access, and competing health priorities, which deter them from seeking eye care services (31). Cultural factors also play a role, as countries like United States, Australia, Ghana and Nigeria may benefit from more robust community outreach programs and public awareness campaigns about eye health, encouraging earlier detection and treatment, while some Ethiopian communities may rely on traditional healing practices or have lower awareness of the importance of eye care, leading to lower utilization rates until vision problems become more severe (32). All these aspects highlight the vital role of healthcare accessibility, socioeconomic conditions, and cultural awareness in shaping ECSU rates, emphasizing the need for targeted interventions to improve ECSU, particularly in underserved regions.
In the multivariable multi-level logistic regression; age, health insurance, distance to the nearest eye care facility, and awareness about regular eye check-ups were significantly associated with ECSU. Consistent with different studies conducted in Abuja, Nigeria, South Korea, Tehran, Australia, and America (21, 26, 28, 33–35), Individuals in the age group of 65 and above had higher odds of ECSU as compared to their counterparts. This might be because, as people age, eye conditions like cataracts, macular degeneration, glaucoma, and presbyopia become more prevalent and pronounced. Additionally, older adults are more susceptible to chronic health conditions such as hypertension and diabetes, which can have harmful effects on their vision. As a result, regular eye exams are essential not only for early detection but also for managing these age-related eye health concerns effectively (36).
Health insurance is a factor for ECSU in which, Participants who have health insurance had higher odds of ECSU as compared to their counterparts. This finding is supported by a study done in the United States (37). This might be because health insurance makes eye care services more accessible by reducing financial barriers, covering routine exams, prescription eyewear, treatments, and emergency care. With these services within reach, individuals are more likely to prioritize their eye health and seek timely care when needed.
In this study, participants living near to eye care facility had higher odds of ECSU as compared to their counterparts. This finding was supported by a study done in western Kenya (38). This could be because the proximity of eye care facilities enhances convenience, reduces transportation obstacles, and fosters greater awareness and trust. All of these factors contribute to higher utilization rates among individuals living closer to these facilities.
Consistent with studies done in Hawassa and Australia (9, 28), participants who were aware of regular eye checkups had higher odds of ECSU as compared to their counterparts. The reason might be due to awareness fosters a proactive approach to eye health. Educated individuals understand the importance of routine exams and the early detection of potential issues. This knowledge encourages them to seek timely care, leading to increased utilization.
Unlike previous studies conducted in urban or high-income settings with well-established healthcare infrastructures, our study provides novel insights into eye care service utilization in a low-resource rural Ethiopian context, where unique structural and socioeconomic barriers exist. In Andabet, limited eye care facilities, long travel distances, low health insurance coverage, and poor awareness about regular eye check-ups significantly hinder access to care. Ethiopia’s community-based health insurance (CBHI) is still in its early stages, and its role in improving eye care access remains underexplored. Additionally, the cultural perception of eye diseases, lower literacy rates, and delayed healthcare-seeking behavior in this setting differ from populations studied in high-income countries, where preventive eye care is more common. Also, unlike previous rural-based Ethiopian studies that use the traditional regression model, our study applies a multi-level mixed-effect analysis, which accounts for both individual-level and community-level factors influencing eye care utilization. This approach captures variations at different levels (household, community, healthcare system), providing a more comprehensive understanding of access barriers. The multi-level approach also helps to reduce cluster-level confounding bias, intraclass correlation bias, and aggregation bias, ensuring more reliable and robust findings.
Strengths and limitations of the study
There were strengths and foibles in this study. To begin with the strength, the study exploits multi-level mixed effect modeling taking into account the clustering effect to draw valid inferences and conclusions. Moreover, to ascertain representativeness, the study uses an adequate sample size. However, this study had limitations: As it’s a cross-sectional study, it may not exhibit a true temporal relationship between the outcome and the independent variables. Besides Social desirability bias might be introduced while assessing sensitive variables. Future research should focus on identifying additional barriers to eye care service utilization in Ethiopia, exploring the impact of socioeconomic factors, and evaluating the effectiveness of targeted interventions aimed at improving access to and awareness of eye care services.
Conclusion
In this study, the magnitude of ECSU was lower than in other studies. Age, health insurance, distance to the nearest eye care facility, and awareness about regular eye check-ups were independent determinants of ECSU. These findings underscore the urgent need for policy-driven interventions to improve access and ensure fair distribution of eye care services. Therefore, policymakers should focus on strengthening health insurance enrollment and ensuring its accessibility for all, particularly in rural communities. They must also invest in strategically expanding eye care facilities to reduce geographic disparities and integrate routine eye examinations into primary healthcare services. Additionally, large-scale public awareness campaigns are crucial to foster a culture of preventive eye care. A well-coordinated, multi-sectoral policy approach centered on accessibility, integration, and education is imperative to improving eye care utilization and reducing the burden of vision impairment.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Debre Tabor University, Health Science College (Reference Number: 1099). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ST: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing. TM: Data curation, Project administration, Software, Writing – original draft, Writing – review & editing. GT: Project administration, Software, Supervision, Writing – original draft, Writing – review & editing. DD: Data curation, Software, Validation, Writing – original draft, Writing – review & editing. BB: Investigation, Supervision, Writing – original draft, Writing – review & editing. SA: Investigation, Project administration, Writing – original draft, Writing – review & editing. BS: Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. FD: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at:
Supplementary Table S1 | Data set.
References
1. Carrasquillo O. Health care utilization. Encycl Behav Med. (2013) 22:1001–2.
Google Scholar
2. Berhane Y, Worku A, Bejiga A, Adamu L, Alemayehu W, Bedri A, et al. Prevalence and causes of blindness and low vision in Ethiopia. Ethiop J Health Dev. (2007) 21:204–10. doi: 10.4314/ejhd.v21i3.10050
Crossref Full Text | Google Scholar
3. Ehrlich JR, Ndukwe T, Solway E, Woodward MA, Singer DC, Newman-Casey PA, et al. Self-reported eye care use among US adults aged 50 to 80 years. JAMA Ophthalmol. (2019) 137:1061–6. doi: 10.1001/jamaophthalmol.2019.1927
PubMed Abstract | Crossref Full Text | Google Scholar
5. Vela C, Samson E, Zunzunegui MV, Haddad S, Aubin M-J, Freeman EE. Eye care utilization by older adults in low, middle, and high income countries. BMC Ophthalmol. (2012) 12:1–7. doi: 10.1186/1471-2415-12-5
PubMed Abstract | Crossref Full Text | Google Scholar
6. Assaye AK, Tegegn MT, Belete GT. Eye care utilization among older subjects with visual impairment in Northwest Ethiopia. J Ophthalmic Vis Res. (2023) 18:306. doi: 10.18502/jovr.v18i3.13779
PubMed Abstract | Crossref Full Text | Google Scholar
7. Alemu T, Seyum D, Gebre M, Sisay A, Sorato MM. Level of eye healthcare utilisation and associated factors in Gamo and Gofa Zones, Southern Ethiopia: a community-based, cross-sectional study. BMJ Open. (2024) 14:e082612. doi: 10.1136/bmjopen-2023-082612
PubMed Abstract | Crossref Full Text | Google Scholar
8. Bekele MM, Shumye AF, Tegegn MT. Eye care service utilization and associated factors among adults in Debre Berhan Town, North Shewa, Ethiopia, 2023. Front Public Health. (2024) 12:1440357. doi: 10.3389/fpubh.2024.1440357
PubMed Abstract | Crossref Full Text | Google Scholar
9. Morka ED, Yibekal BT, Tegegne MM. Eye care service utilization and associated factors among older adults in Hawassa city, South Ethiopia. PLoS ONE. (2020) 15:e0231616. doi: 10.1371/journal.pone.0231616
PubMed Abstract | Crossref Full Text | Google Scholar
11. Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Jones I, et al. The economics of vision impairment and its leading causes: a systematic review. EClinicalMedicine. (2022) 46:101354. doi: 10.1016/j.eclinm.2022.101354
PubMed Abstract | Crossref Full Text | Google Scholar
12. Vanderpuye I, Nyame I, Okai M-P. Challenges inherent in the academic endeavours of students with visual impairment. Int J Inclus Educ. (2024) 28:1954–67. doi: 10.1080/13603116.2022.2036830
Crossref Full Text | Google Scholar
13. Chuck RS, Dunn SP, Flaxel CJ, Gedde SJ, Mah FS, Miller KM, et al. Comprehensive adult medical eye evaluation preferred practice pattern®. Ophthalmology. (2021) 128:P1–P29. doi: 10.1016/j.ophtha.2020.10.024
PubMed Abstract | Crossref Full Text | Google Scholar
14. Yusufu M, Bukhari J, Yu X, Lin TP, Lam DS, Wang N. Challenges in eye care in the Asia-Pacific region. Asia Pac J Ophthalmol. (2021) 10:423–9. doi: 10.1097/APO.0000000000000391
PubMed Abstract | Crossref Full Text | Google Scholar
15. Sengo DB, Marraca NA, Muaprato AM, García-Sanjuan S, Caballero P, López-Izquierdo I. Barriers to accessing eye health services in suburban communities in Nampula, Mozambique. Int J Environ Res Public Health. (2022) 19:3916. doi: 10.3390/ijerph19073916
PubMed Abstract | Crossref Full Text | Google Scholar
16. Bourne RR, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. (2017) 5:e888–e97. doi: 10.1016/S2214-109X(17)30293-0
PubMed Abstract | Crossref Full Text | Google Scholar
17. Ocansey S, Kumi-Kyereme A, Awusabo-Asare K, Ilechie AA, Boadi-Kusi SB, Abraham CH. Utilization of eye care services among Ghanaian elderly population: evidence from a peri-urban community. Am Orthopt J. (2013) 2:123. doi: 10.9734/OR/2013/5543
Crossref Full Text | Google Scholar
18. Yirga GK, Bantie B, Hiruy EG, Baye AA, Kerebeh G, Shiferaw K, et al. Health checkup practice and its associated factors among adults in South Gondar zone Ethiopia. Sci Rep. (2024) 14:21237. doi: 10.1038/s41598-024-69921-3
PubMed Abstract | Crossref Full Text | Google Scholar
19. Kifle M, Mbarika VW, Datta P. Telemedicine in sub-Saharan Africa: the case of teleophthalmology and eye care in Ethiopia. J Am Soc Inf Sci Technol. (2006) 57:1383–93. doi: 10.1002/asi.20448
Crossref Full Text | Google Scholar
20. Hamed MM, Masoud MA. An exploratory assessment of self-reported satisfaction with infrastructure and out-of-home activities for people with vision impairments. Vision. (2023) 7:58. doi: 10.3390/vision7030058
PubMed Abstract | Crossref Full Text | Google Scholar
21. Olusanya BA, Ashaye AO, Owoaje ET, Baiyeroju AM, Ajayi BG. Determinants of utilization of eye care services in a rural adult population of a developing country. Middle East Afr J Ophthalmol. (2016) 23:96. doi: 10.4103/0974-9233.164621
PubMed Abstract | Crossref Full Text | Google Scholar
22. Hwang J, Rudnisky C, Bowen S, Johnson JA. Socioeconomic factors associated with visual impairment and ophthalmic care utilization in patients with type II diabetes. Can J Ophthalmol. (2015) 50:119–26. doi: 10.1016/j.jcjo.2014.11.014
PubMed Abstract | Crossref Full Text | Google Scholar
24. Adimassu NF, Asefa N, Anibesei D, Belete G. Poor eye care service utilization among adults in Gondar City, Northwest Ethiopia. EC Ophthal. (2018) 9:647–57.
Google Scholar
25. Ilechie AA, Otchere H, Darko-Takyi C, Halladay AC. Access to and utilization of eye care services in Ghana. PLoS ONE. (2013) 21:4.
Google Scholar
26. Ibeneche H, Ekpenyong B, Ebri A. Barriers to accessing eye care services in the federal capital territory, Abuja, Nigeria. J Niger Optom Assoc. (2018) 20:64–9. doi: 10.13140/RG.2.2.24493.74724
Crossref Full Text | Google Scholar
27. Wilson FA, Stimpson JP, Wang Y. Inconsistencies exist in national estimates of eye care services utilization in the United States. J Ophthalmol. (2015) 2015:435606. doi: 10.1155/2015/435606
PubMed Abstract | Crossref Full Text | Google Scholar
28. Foreman J, Xie J, Keel S, Taylor HR, Dirani M. Utilization of eye health-care services in Australia: the national eye health survey. Clin Experiment Ophthalmol. (2018) 46:213–21. doi: 10.1111/ceo.13035
PubMed Abstract | Crossref Full Text | Google Scholar
29. Owusu-Afriyie B, Peter N, Ivihi F, Kopil I, Gende T. Barriers to the uptake of eye care services: a cross-sectional survey from rural and urban communities. PLoS ONE. (2024) 19:e0308294. doi: 10.1371/journal.pone.0308294
PubMed Abstract | Crossref Full Text | Google Scholar
30. Devi GV, Anand B. A review of the determinants that influence the use of eye care servic. Journal of Positive School Psychology. (2022) 6:2992–3000.
Google Scholar
31. Melese M, Alemayehu W, Friedlander E, Courtright P. Indirect costs associated with accessing eye care services as a barrier to service use in Ethiopia. Trop Med Int Health. (2004) 9:426–31. doi: 10.1111/j.1365-3156.2004.01205.x
PubMed Abstract | Crossref Full Text | Google Scholar
32. Solomon SD, Shoge RY, Ervin AM, Contreras M, Harewood J, Aguwa UT, et al. Improving access to eye care: a systematic review of the literature. Ophthalmology. (2022) 129:e114–e26. doi: 10.1016/j.ophtha.2022.07.012
PubMed Abstract | Crossref Full Text | Google Scholar
33. Park YS, Heo H, Ye BJ, Suh Y-W, Kim S-H, Park SH, et al. Prevalence and factors associated with the use of eye care services in South Korea: Korea national health and nutrition examination survey 2010–2012. Korean J Ophthalmol. (2017) 31:58–70. doi: 10.3341/kjo.2017.31.1.58
PubMed Abstract | Crossref Full Text | Google Scholar
34. Fotouhi A, Hashemi H, Mohammad K. Eye care utilization patterns in Tehran population: a population based cross-sectional study. BMC Ophthalmol. (2006) 6:1–5. doi: 10.1186/1471-2415-6-4
PubMed Abstract | Crossref Full Text | Google Scholar
35. Jiang X, Varma R, Torres M, Hsu C, McKean-Cowdin R, Group CAES. Self-reported use of eye care among adult Chinese Americans: the Chinese American eye study. Clin Exp Ophthalmol. (2017) 176:183–93. doi: 10.1016/j.ajo.2017.01.018
PubMed Abstract | Crossref Full Text | Google Scholar
36. Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. (2004) 52:1662–7. doi: 10.1111/j.1532-5415.2004.52458.x
PubMed Abstract | Crossref Full Text | Google Scholar
38. Rono MMed HK, Macleod D, Bastawrous A, Wanjala E, Gichangi M, Burton MJ. Utilization of secondary eye care services in western Kenya. Clin Exp Ophthalmol. (2019) 16:3371. doi: 10.3390/ijerph16183371
PubMed Abstract | Crossref Full Text | Google Scholar
link

