A total of 17 participants were enrolled in the program, with 13 (76.5%) from Nepal and 4 (23.5%) from India. A Google form survey was distributed to all the participants. Of the 17 participants, 15 (88.2%) completed the survey. Response rates varied across hospitals, with two hospitals having 100% participation, while in the other two hospitals, the response rates were 75% (3 out of 4) and 80% (4 out of 5), respectively. Among the participants, 9 (53%) were male, and 10 (59%) were between the ages of 30 and 40. The educational background of the participants included 4 ophthalmologists, and 5 each optometrists and ophthalmic assistants. (Table 1)
Program delivery/knowledge/skills/competency (before and after skilling: before and after score comparison):-
Quantitative
Responses from the participants suggest that the knowledge level improved significantly in all the domains (Table 2). The knowledge level increased on how to conduct a literature review, how to formulate a research question and knowledge of various study designs. However, topics like sample size calculations, data analysis plans, and manuscript writing required additional skilling.
Qualitative
Knowledge improvement and publication success
Overall participants felt that their knowledge improved substantially after joining the program. Two ophthalmologists expressed that their understanding improved a lot and that their respective teams could successfully publish two manuscripts in peer-reviewed journals.
Effective workshop approach, with room for material improvement
Participants appreciated the workshop’s standard and approach, considering it efficient. However, feedback indicated that workshop materials, while generally good, needed further standardization, especially regarding learning formats. The need for more structured and standardized training modules, particularly for beginners, was emphasized. “Should develop standardized training modules, especially for the beginners.” Another participant felt that some of the material was confusing and expressed concern- “I get even more confused after going through the training content when I train my students”. Her suggestion was to revise the program content though she did not provide any specific suggestions.
Need for consistent and long-term mentorship
One participant also mentioned that for their hospital, a frequent change of mentors hampered their work as each mentor differed in their approach which led to confusing signals. This team suggested that the presence of a dedicated mentor for a longer duration might be helpful for them to learn the skills better.
Difficulties with online delivery and suggested solutions
Three participants stated that the online delivery of the program had lots of challenges, especially due to internet connectivity issues. They suggested that the provision of lecture transcripts could be an option to overcome such challenges.
Statistical learning and mentor support
Two participants mentioned that they partially completed the ORCB program as the in-person statistics workshop was attended by two out of four members. One member expressed unhappiness that though they wanted to attend but were not allowed by the hospital administration. The person requested that “Next time when Seva/IIPH-H organize such an event, they can consider calling all members instead of a few of them.” One person mentioned that learning from the program was minimal as he/she did not learn any additional statistical concepts. Some participants opined that they were not confident in responding to the comments of reviewers on statistics when they submitted a manuscript and had to approach the team mentor from the training institution to respond to the same. Unfortunately, this respondent did not share this concern with the designated team mentor from the training institution as he/she felt demotivated as adequate statistical analytical skills were not picked up.
Need for incorporating health economics
While acknowledging the program’s strengths, participants identified challenges, particularly in the areas of cost-effectiveness and health economics. One participant expressed “Despite the strengths, the program faced challenges in topics such as cost-effectiveness and health economics within the hospital.” They suggested that incorporating a health economics component into the projects could address the hospital authorities’ concerns about financial sustainability.
Practices in the hospital after skilling
Quantitative
While 66.7% (n = 10) of participants were involved in designing study protocol development, 73.3% (n = 11) participants took part in data analysis at their hospital (Either analysis of routine data, research data, or both). Importantly, 60% (n = 9) of participants trained other hospital staff or students on topics they learnt during the training program. (Table 3) Most of their training was related to literature search (n = 7; 77.8%) formulating research questions and objectives (n = 8; 88.9%) and designing tools for data collection (n = 5; 55.6%). Most of the training for the hospital students and staff was related to these areas. (Table 4)
Qualitative
Positive impact on hospital services and operational practices
The overall improvement of the hospital services had been promising after the training. One participant expressed that “Significant changes have been observed in the research and operation aspects.” The approach to work now involves a combination of learning, research, and operational activities. The software for electronic hospital records was updated to facilitate seamless integration with routine work. Also, efforts have been made to improve the connections between the patients from vision centres and base hospitals based on the learning from the training program.
Potential for self-learning within hospitals
Another participant from the same team who works in the clinical lab felt that there was tremendous scope for self-learning at the hospital as a large amount of data was available in the different departments of the hospital. “One participant mentioned having improved a lot in designing studies and manuscript writing based on the fundamental principles learnt from the training program”.
Internal training initiatives
Nine participants took the initiative to train additional teams within the hospital. This internal training covered topics such as proposal writing, data management, analysis, and scientific writing, indicating a positive ripple effect of the original training program.
Necessity of building a dedicated research team
Participants emphasized the importance of research in improving hospital services. However, they noted that research efforts were often driven by individual clinicians rather than a coordinated team. One participant expressed – “Building a team of researchers who constantly work on the research flow and its outcome is critical rather than only clinicians spending time as they are quite busy. Unfortunately, it is all about the individual approach and not a team approach.”
Insufficient time for implementation
One participant expressed a concern that -“The short time for implementation adds pressure, impacting the program’s overall effectiveness”. This highlights the need for better time management.
Gaps in research dissemination and accountability
Despite the progress in research activities, one participant informed that there is a lack of formal systems for disseminating research findings within the hospital. Although verbal updates were provided to hospital authorities 3–4 times a year, there is no provision for documented formal meetings to keep track of the action plans. Also, when researchers at our hospital publish any paper, there is no system to disseminate the findings among the other stakeholders.
Motivators and challenges
Quantitatiive (n = 15)
Figure 1: Motivating factors/enablers and challenges faced by participants. This figure presents the quantitative analysis of the primary motivators and challenges reported by participants in the ORCB program. Notably, the highest scores reflect significant improvements in factors that contribute to effective research practices. Major challenges identified include the absence of institutional incentives, additional funding for research provided by the hospital, workload management by the hospital authority and no provision of statistical software for analysis. Conversely, self-motivation, coordination among the research team and time management by self were the major enablers.
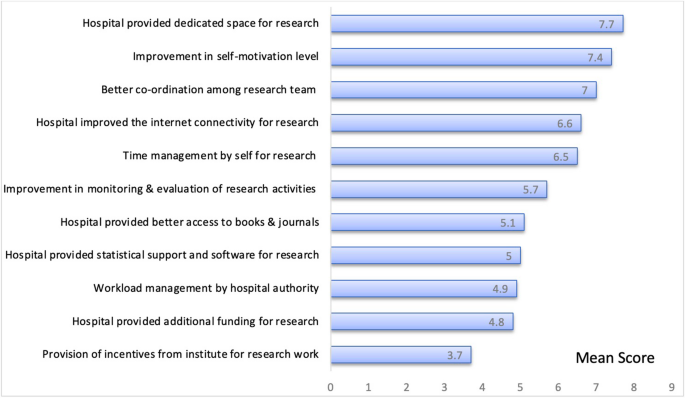
Mean score of motivating factors/enablers and challenges among participants
Qualitative
Need for enhanced statistical tools and software
Participants discussed the importance of using robust statistical software for data analysis. One participant opined “Increase the use of statistical tools like Stata software for more robust analysis.” One participant expressed he/she was directly involved in guiding students’ (postgraduates) research. “I guide 3–4 postgraduates every year as a part of my job and I guide them for their thesis work. So, it is a routine process for me”. Two other participants mentioned that they had received a few of the thesis protocols from the students for review. Both were guiding optometrists for their thesis. Lack of a licensed version of the software at the hospitals also demotivates them- “We learned the basics during the training, but because we do not have licensed software for data analysis like SPSS or Stata software, we are handicapped in doing that. The hospital administration can help us in getting that.”
Balancing clinical work and research
Balancing clinical work and research was identified as a major challenge, particularly for clinicians. “Conducting research and clinical work is a double burden for us when management wants us to work on research without reducing our clinical workload”.
Lack of incentive for research
For clinicians, motivators like research work will add to their resumes and help in promotion. Nothing much of an incentive is there for the research work.
link

