Progress on the Sustainable Development Goals: The Gender Snapshot 2023 (UN Women and United Nations Department of Economic and Social Affairs, 2023).
Patwardhan, V. et al. Differences across the lifespan between females and males in the top 20 causes of disease burden globally: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Public Health 9, e282–e294 (2024).
Google Scholar
Stall, N. M., Shah, N. R. & Bhushan, D. Unpaid family caregiving—the next frontier of gender equity in a postpandemic future. JAMA Health Forum 4, e231310 (2023).
Google Scholar
Sex, gender, and the cost of neurological disorders. Lancet Neurol. 22, 367 (2023).
Measures of Early-Life Brain Health at Population Level: Report of a Technical Meeting (WHO, 2023).
Optimizing Brain Health Across the Life Course: WHO Position Paper (WHO, 2022).
Winter, S. F. et al. National plans and awareness campaigns as priorities for achieving global brain health. Lancet Glob. Health 12, e697–e706 (2024).
Google Scholar
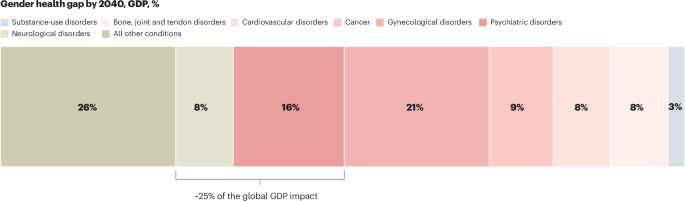
Ellingrud, K., Pérez, L., Petersen, A. & Sartori, V. Closing the Women’s Health Gap: A $1 Trillion Opportunity to Improve Lives and Economies (McKinsey & Company, 2024); https://www.mckinsey.com/mhi/our-insights/closing-the-womens-health-gap-a-1-trillion-dollar-opportunity-to-improve-lives-and-economies#/
Deady, M. et al. The impact of depression, anxiety and comorbidity on occupational outcomes. Occup. Med. 72, 17–24 (2022).
Google Scholar
Smith, E. et al. A brain capital grand strategy: toward economic reimagination. Mol. Psychiatry 26, 3–22 (2021).
Google Scholar
Eyre, H. A., Hynes, W., Ayadi, R., Manes, F. & Swieboda, P. Brain capital is crucial for global sustainable development. Lancet Neurol. 23, 233–235 (2024).
Google Scholar
McGrath, J. J. et al. Age of onset and cumulative risk of mental disorders: a cross-national analysis of population surveys from 29 countries. Lancet Psychiatry 10, 668–681 (2023).
Google Scholar
Steinmetz, J. D. et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 23, 344–381 (2024).
Heidari, S., Babor, T. F., De Castro, P., Tort, S. & Curno, M. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res. Integr. Peer Rev. 1, 2 (2016).
Google Scholar
Madsen, T. E. et al. Sex- and gender-based medicine: the need for precise terminology. Gend. Genome (2017).
Hyde, J. S., Bigler, R. S., Joel, D., Tate, C. C. & van Anders, S. M. The future of sex and gender in psychology: five challenges to the gender binary. Am. Psychol. 74, 171–193 (2019).
Google Scholar
GBD Results (IHME, 2021); https://vizhub.healthdata.org/gbd-results/
Nussbaum, N. L. ADHD and female specific concerns. J. Atten. Disord. 16, 87–100 (2012).
Google Scholar
Attoe, D. E. & Climie, E. A. Miss. Diagnosis: a systematic review of ADHD in adult women. J. Atten. Disord. 27, 645–657 (2023).
Google Scholar
Ferretti, M. T. et al. Sex differences in Alzheimer disease—the gateway to precision medicine. Nat. Rev. Neurol. 14, 457–469 (2018).
Woolley, C. S. His and hers: sex differences in the brain. Cerebrum 2021, cer-02-21 (2021).
Google Scholar
Hentzen, N. B. et al. Mapping of European activities on the integration of sex and gender factors in neurology and neuroscience. Eur. J. Neurol. 29, 2572–2579 (2022).
Google Scholar
Kundakovic, M. & Rocks, D. Sex hormone fluctuation and increased female risk for depression and anxiety disorders: from clinical evidence to molecular mechanisms. Front. Neuroendocrinol. 66, 101010 (2022).
Google Scholar
Roeder, H. J. & Leira, E. C. Effects of the menstrual cycle on neurological disorders. Curr. Neurol. Neurosci. Rep. 21, 34 (2021).
Google Scholar
Handy, A. B., Greenfield, S. F., Yonkers, K. A. & Payne, L. A. Psychiatric symptoms across the menstrual cycle in adult women: a comprehensive review. Harv. Rev. Psychiatry 30, 100–117 (2022).
Google Scholar
McCarthy, M. M. Sex differences in the developing brain as a source of inherent risk. Dialogues Clin. Neurosci. 18, 361–372 (2016).
Google Scholar
McCarthy, M. M. Multifaceted origins of sex differences in the brain. Phil. Trans. R. Soc. B 371, 20150106 (2016).
Google Scholar
McCarthy, M. M., Arnold, A. P., Ball, G. F., Blaustein, J. D. & De Vries, G. J. Sex differences in the brain: the not so inconvenient truth. J. Neurosci. 32, 2241–2247 (2012).
Google Scholar
Quintana, G. R. & Pfaus, J. G. Do sex and gender have separate identities? Arch. Sex. Behav. 53, 2957–2975 (2024).
Google Scholar
Baez, S., Castro-Aldrete, L., Britton, G., Ibañez, A. & Santuccione-Chadha, A. Enhancing brain health in the Global South through a sex and gender lens. Nat. Ment. Health (2024).
Google Scholar
Ruigrok, A. N. V. et al. A meta-analysis of sex differences in human brain structure. Neurosci. Biobehav. Rev. 39, 34–50 (2014).
Google Scholar
Giedd, J. N., Raznahan, A., Mills, K. L. & Lenroot, R. K. Review: magnetic resonance imaging of male/female differences in human adolescent brain anatomy. Biol. Sex Differ. 3, 19 (2012).
Google Scholar
Kang, H. J. et al. Spatio-temporal transcriptome of the human brain. Nature 478, 483–489 (2011).
Google Scholar
Wingo, A. P. et al. Sex differences in brain protein expression and disease. Nat. Med. 29, 2224–2232 (2023).
Google Scholar
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446 (2020).
Google Scholar
Mazure, C. M. & Jones, D. P. Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Womens Health 15, 94 (2015).
Google Scholar
Castro-Aldrete, L. et al. Sex and gender considerations in Alzheimer’s disease: the Women’s Brain Project contribution. Front. Aging Neurosci. 15, 1105620 (2023).
Google Scholar
Maleki, N. et al. Her versus his migraine: multiple sex differences in brain function and structure. Brain 135, 2546–2559 (2012).
Google Scholar
Eisenstein, M. Closing the gender gap in migraine research. Nature 586, S16–S17 (2020).
Google Scholar
Liu, J. et al. Gender-related differences in the dysfunctional resting networks of migraine suffers. PLoS ONE 6, e27049 (2011).
Google Scholar
Granella, F. et al. Migraine without aura and reproductive life events: a clinical epidemiological study in 1300 women. Headache 33, 385–389 (1993).
Google Scholar
Delaruelle, Z. et al. Male and female sex hormones in primary headaches. J. Headache Pain 19, 117 (2018).
Google Scholar
Vetvik, K. G., MacGregor, E. A., Lundqvist, C. & Russell, M. B. Prevalence of menstrual migraine: a population-based study. Cephalalgia 34, 280–288 (2014).
Google Scholar
Clayton, J. A. Sex influences in neurological disorders: case studies and perspectives. Dialogues Clin. Neurosci. 18, 357–360 (2016).
Google Scholar
Petersen, A., Pérez, L., Herbig, B. & Tatwawadi, P. Bridging the Womens Health Gap: A Country-Level Exploration (McKinsey & Company, 2024); https://www.mckinsey.com/mhi/our-insights/bridging-the-womens-health-gap-a-country-level-exploration
Arenaza-Urquijo, E. M. et al. Sex and gender differences in cognitive resilience to aging and Alzheimer’s disease. Alzheimers Dement. 20, 5695–5719 (2024).
Google Scholar
Ferretti, M. T. et al. Sex and gender differences in Alzheimer’s disease: current challenges and implications for clinical practice. Eur. J. Neurol. 27, 928–943 (2020).
Google Scholar
Rosende-Roca, M. et al. The role of sex and gender in the selection of Alzheimer patients for clinical trial pre-screening. Alzheimers Res. Ther. 13, 95 (2021).
Google Scholar
Mielke, M. M. Sex and gender differences in Alzheimer’s disease dementia. Psychiatr. Times 35, 14–17 (2018).
Google Scholar
Rahman, A. et al. Sex and gender driven modifiers of Alzheimer’s: the role for estrogenic control across age, race, medical, and lifestyle risks. Front. Aging Neurosci. 11, 315 (2019).
Google Scholar
Pletzer, B., Harris, T.-A., Scheuringer, A. & Hidalgo-Lopez, E. The cycling brain: menstrual cycle related fluctuations in hippocampal and fronto-striatal activation and connectivity during cognitive tasks. Neuropsychopharmacology 44, 1867–1875 (2019).
Google Scholar
Avila-Varela, D. S. et al. Whole-brain dynamics across the menstrual cycle: the role of hormonal fluctuations and age in healthy women. NPJ Womens Health 2, 8 (2024).
Google Scholar
Zsido, R. G. et al. Ultra-high-field 7T MRI reveals changes in human medial temporal lobe volume in female adults during menstrual cycle. Nat. Ment. Health 1, 761–771 (2023).
Google Scholar
Nerattini, M. et al. Systematic review and meta-analysis of the effects of menopause hormone therapy on risk of Alzheimer’s disease and dementia. Front. Aging Neurosci. 15, 1260427 (2023).
Google Scholar
Taylor, C. M., Pritschet, L. & Jacobs, E. G. The scientific body of knowledge—whose body does it serve? A spotlight on oral contraceptives and women’s health factors in neuroimaging. Front. Neuroendocrinol. 60, 100874 (2021).
Google Scholar
Jacobs, E. G. Only 0.5% of neuroscience studies look at women’s health. Here’s how to change that. Nature 623, 667 (2023).
Google Scholar
Inkster, A. M., Wong, M. T., Matthews, A. M., Brown, C. J. & Robinson, W. P. Who’s afraid of the X? Incorporating the X and Y chromosomes into the analysis of DNA methylation array data. Epigenetics Chromatin 16, 1 (2023).
Google Scholar
Wise, A. L., Gyi, L. & Manolio, T. A. eXclusion: toward Integrating the X chromosome in genome-wide association analyses. Am. J. Hum. Genet. 92, 643–647 (2013).
Google Scholar
Leitão, E. et al. Systematic analysis and prediction of genes associated with monogenic disorders on human chromosome X. Nat. Commun. 13, 6570 (2022).
Google Scholar
MacGregor, E. A. Migraine, menopause and hormone replacement therapy. Post Reprod. Health 24, 11–18 (2018).
Google Scholar
Tasca, C., Rapetti, M., Carta, M. G. & Fadda, B. Women and hysteria in the history of mental health. Clinic. Pract. Epidemiol. Ment. Health 8, 110–119 (2012).
Google Scholar
Tu, H.-F., Skalkidou, A., Lindskog, M. & Gredebäck, G. Maternal childhood trauma and perinatal distress are related to infants’ focused attention from 6 to 18 months. Sci. Rep. 11, 24190 (2021).
Google Scholar
Scheinost, D., Spann, M. N., McDonough, L., Peterson, B. S. & Monk, C. Associations between different dimensions of prenatal distress, neonatal hippocampal connectivity, and infant memory. Neuropsychopharmacology 45, 1272–1279 (2020).
Google Scholar
Armstrong, C. ACOG guidelines on psychiatric medication use during pregnancy and lactation. Am. Fam. Physician 78, 772–778 (2008).
Liu, C., Pace, S., Bromley, R. & Dobson, R. Exposure to medication for neurological disease in pregnancy—time to consider the long-term implications? EClinicalMedicine 63, 102157 (2023).
Google Scholar
Todd, C., Lagman-Bartolome, A. M. & Lay, C. Women and migraine: the role of hormones. Curr. Neurol. Neurosci. Rep. 18, 42 (2018).
Google Scholar
Anglin, D. M., Alberti, P. M., Link, B. G. & Phelan, J. C. Racial differences in beliefs about the effectiveness and necessity of mental health treatment. Am. J. Community Psychol. 42, 17–24 (2008).
Google Scholar
Nelson, T., Shahid, N. N. & Cardemil, E. V. Do I really need to go and see somebody? Black women’s perceptions of help-seeking for depression. J. Black Psychol. 46, 263–286 (2020).
Chisholm, D. et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry 3, 415–424 (2016).
Google Scholar
Krivkovich, A., Field, E., Yee, L., McConnell, M. & Smith, H. Women in the Workplace (McKinsey & Company, 2023); https://www.mckinsey.com/featured-insights/diversity-and-inclusion/women-in-the-workplace
Farina, F. R. et al. Young adult brain capital: a new opportunity for dementia prevention. J. Alzheimers Dis. 94, 415–423 (2023).
Google Scholar
Dawson, W. D. et al. Investing in late-life brain capital. Innov. Aging 6, igac016 (2022).
Google Scholar
Gotlib, I. H., Joormann, J. & Foland-Ross, L. C. Understanding familial risk for depression: a 25-year perspective. Perspect. Psychol. Sci. 9, 94–108 (2014).
Google Scholar
2023 Alzheimer’s disease facts and figures. Alzheimers Dement. 19, 1598–1695 (2023).
Pallier, P. N. et al. Chromosomal and environmental contributions to sex differences in the vulnerability to neurological and neuropsychiatric disorders: implications for therapeutic interventions. Prog. Neurobiol. 219, 102353 (2022).
Google Scholar
Vinogradova, Y. et al. Use of menopausal hormone therapy and risk of dementia: nested case-control studies using QResearch and CPRD databases. Br. Med. J. 374, n2182 (2021).
Google Scholar
Report of the Advisory Committee on Research on Women’s Health: Fiscal Years 2019–2020 (Office of Research on Women’s Health, 2021).
Ma, M., Dorstyn, D., Ward, L. & Prentice, S. Alzheimers’ disease and caregiving: a meta-analytic review comparing the mental health of primary carers to controls. Aging Ment. Health 22, 1395–1405 (2018).
Google Scholar
Sheehan, O. C. et al. Stress, burden, and well-being in dementia and nondementia caregivers: insights from the caregiving transitions study. Gerontologist 61, 670–679 (2021).
Google Scholar
Ibáñez, A. et al. Dementia caregiving across Latin America and the Caribbean and brain health diplomacy. Lancet Healthy Longev. 2, e222–e231 (2021).
Google Scholar
Liu, R., Chi, I. & Wu, S. Caregiving burden among caregivers of people with dementia through the lens of intersectionality. Gerontologist 62, 650–661 (2022).
Google Scholar
Xiong, C. et al. Sex and gender differences in caregiving burden experienced by family caregivers of persons with dementia: a systematic review. PLoS ONE 15, e0231848 (2020).
Google Scholar
Arbel, I., Bingham, K. S. & Dawson, D. R. A scoping review of literature on sex and gender differences among dementia spousal caregivers. Gerontologist 59, e802–e815 (2019).
Google Scholar
Abken, E., Ferretti, M. T., Castro-Aldrete, L., Santuccione Chadha, A. & Tartaglia, M. C. The impact of informant-related characteristics including sex/gender on assessment of Alzheimer’s disease symptoms and severity. Front. Glob. Womens Health 5, 1326881 (2024).
Google Scholar
Brassey, J., Herbig, B., Jeffery, B. & Ungerman, D. Reframing Employee Health: Moving Beyond Burnout to Holistic Health (McKinsey & Company, 2024); https://www.mckinsey.com/mhi/our-insights/reframing-employee-health-moving-beyond-burnout-to-holistic-health
Integrated Results and Resources Framework (IRRF) of UN-Women Strategic Plan (UN Women, 2022); https://www.unwomen.org/sites/default/files/Headquarters/Attachments/Sections/Library/Publications/2021/UN-Women-Strategic-Plan-2022-2025-Annex-01-Integrated-results-and-resources-framework-en.pdf
International Classification of Diseases Eleventh Revision (ICD-11) (WHO, 2022).
Owolabi, M. O. et al. Global synergistic actions to improve brain health for human development. Nat. Rev. Neurol. 19, 371–383 (2023).
Google Scholar
Ibanez, A. & Zimmer, E. R. Time to synergize mental health with brain health. Nat. Ment. Health 1, 441–443 (2023).
Google Scholar
McKinsey Health Institute. Brain Health https://www.mckinsey.com/mhi/focus-areas/brain-health
Eyre, H. A. et al. Building brain capital. Neuron 109, 1430–1432 (2021).
Google Scholar
Crenshaw, K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 43, 1241 (1991).
Google Scholar
Lock, S. L., Chura, L. R., Dilworth-Anderson, P. & Peterson, J. Equity across the life course matters for brain health. Nat. Aging 3, 466–468 (2023).
Google Scholar
Ungerman, D. et al. How to Achieve Great Health for All? Start in Your City (McKinsey & Company, 2024); https://www.mckinsey.com/mhi/our-insights/how-to-achieve-great-health-for-all-start-in-your-city
Lange, K. W. Task sharing in psychotherapy as a viable global mental health approach in resource-poor countries and also in high-resource settings. Glob. Health J. (2021).
Raviola, G., Naslund, J. A., Smith, S. L. & Patel, V. Innovative models in mental health delivery systems: task sharing care with non-specialist providers to close the mental health treatment gap. Curr. Psychiatry Rep. (2019).
link